Day 1 :
Keynote Forum
Brankica Vasiljevic
NMC Royal Hospital DIP, UAE
Keynote: Kangaroo care in neonatal intensive care

Biography:
Brankica Vasiljevic is the Head of Maternity and Child Health Services in NMC Royal Hospital DIP in Dubai, UAE. After completing her MD, she had completed her clinical postgraduate education (Pediatric and after that Neonatology fellowship) and academic postgraduate education (MSc in Pediatric and Ultrasonography field and PhD in Neonatology field) at Belgrade University School of Medicine in Belgrade, Serbia. She also completed Safety, Quality, Informatics and Leadership Program at Harvard Medical School in Boston, USA. She had won the ESPNIC Educational Grant at 5th World Congress on Pediatric Intensive & Critical Care in Geneva Switzerland (2007). She was a local coordinator for International Neonatal Immunotherapy Study-INIS for Serbia and Montenegro and participated in SIOP 93-01 Study, ITP Study and Twin Birth Study. She has published more than 35 international publications in international indexed journals (100 citations), 5 chapters in various fields of neonatal medicine and has more than 30 presentations in international conferences. She is a Member of Editorial Board of different international journals.
Abstract:
Introduction: Kangaroo Care (KC) or Kangaroo Mother Care (KMC) was introduced more than 25 years ago in Bogota, Colombia, as an alternative to conventional Neonatal Intensive Care Unit (NICU) care for low-birthweight infants in resourcelimited settings. In developing countries, KC for low-birthweight infants has been shown to reduce mortality, severe illness, infection and length of hospital stay. Practice of skin-to-skin contact between the preterm infant and parent KC has been adopted in many NICUs, initially as a means of promoting maternal-infant bonding and breastfeeding. KC is most often offered for stable preterm infants who are 30 weeks’ gestational age at birth, but nowadays KC is offered also to infants on ventilator and extreme preterm infant 26 weeks’ gestational age at birth.
Aim: To examine first the literature and guidelines for KC in very premature infants (<32 weeks) in NICU and after that application and barriers of KC in our NICU.
Result: KC in preterm and sick infants in NICU has benefit in physiological stability (thermoregulation, cardiorespiratory) stability, behavioral (sleep, breastfeeding duration and degree of exclusivity) domains, better nutrition, earlier discharge from hospital and increase parental satisfaction. Barriers to implementation of KC include lack of staff and time, poor knowledge and inadequate training staff and parents, medical concerns including the unstable clinical condition of the newborn or mother, lack of privacy and parental reluctance.
Conclusion: KC facilitates bonding and may improve infant nutrition and neurodevelopment and reduced neonatal morbidity and mortality and decrease length of hospital stay and should therefore be encouraged in clinical practice. Identification of barriers to implementation KC is an important step in the successful implementation.
Keynote Forum
Anupam Gupta
Saint Mary’s Hospital, UK
Keynote: Higher or lower tidal volume: An eternal dilemma!

Biography:
Anupam Gupta is a Consultant Neonatologist at Saint Mary’s Hospital, Manchester UK. He have trained and worked in world famous and prestigious pediatric and neonatal centres in India and UK and developed an expertise in neonatal ventilation and research. He was awarded his PhD by Durham University and he has carried out award winning projects and presented in prestigious international conferences like PAS, EAPS, ESPID, UENPS and helped to organize neonatal conferences here in the UK.
Abstract:
Introduction: Preterm infants often require mechanical ventilation. Volume targeted ventilation has been shown to reduce both complications and the duration of mechanical ventilation. Recommended tidal volume varies from 4-8 mL/kg, but the optimal tidal volume remains elusive.
Aim: To compare a lower (4-5 mL/kg) to a higher (7-8 mL/kg) tidal volume during Volume Guarantee ventilation (VG) of Respiratory Distress Syndrome (RDS) in very preterm infants.
Method: The randomized trial was conducted at North Tees Hospital from 2013-2016. Babies <32 weeks’ gestation or <1500 grams birthweight and requiring mechanical ventilation within 12 hours of life from RDS were included in the study. Babies were randomized to receive lower (4-5 mL/kg) or higher (7-8 mL/kg) tidal volume using VG. The dead space was kept consistent by using standardized trimming of the ET tube. Subjects all received surfactant and were managed by a strict protocol with rescue by high frequency ventilation for defined criteria. The primary outcome was the time to achieve a 25% reduction from the initial Peak Inspiratory Pressure (PIP). Secondary outcomes included the duration of mechanical ventilation, as well as respiratory and nonrespiratory complications. The data were analyzed using SPSS® version 20.0.
Result: During the study period, 70 of 97 (72%) eligible infants were enrolled. The groups were similar (Table 1). The primary outcome, time to reduce PIP (median [IQR]) were 13.6 (8.8-25.2) hours and 17.4 (7.7-27.8) hours, respectively, for higher and lower Vt (p=0.678). The total duration of ventilation (median [IQR]) on higher vs. lower tidal volume was 33.3 (22-368.8) and 61.8 (15.4-177.5) hours, respectively (p=0.959). There were no differences between the two groups for respiratory and non-respiratory complications of prematurity (Table 2).
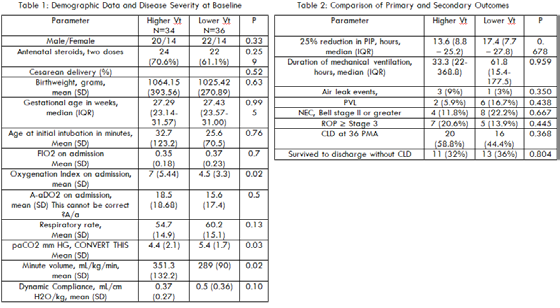
Conclusion: This study failed to find differences in lower versus higher tidal volume delivery in a small population of infants with RDS. It is possible that both tidal volume ranges selected for study are at functional residual capacity.
Keynote Forum
Nasser Ezzat Elshahat Mohamed
Sheikh Khalifa Medical City, UAE
Keynote: Lung ultrasound in pediatrics

Biography:
Nasser Ezzat Elshahat Mohamed has almost 30 years of experience as Neonatologist and Pediatric intensivist. He has graduated with MBBCh in 1989 from Zagazig University, Faculty of Medicine Egypt. He has obtained his Master’s degree of Pediatrics in 1994, Egypt then was moved to work in Kuwait where he spent 20 years working between NICU and PICU, Mubark Al-Kabeer University Hospital. In 2015, he joined Sheikh Khalifa Medical City, PICU managed by Cleveland Clinic in Abu Dhabi as Pediatric Intensivist. He has completed MRCPCH degree in UK and now having Membership of Royal College of Pediatric and Child Health from 2016. He is currently a Senior Consultant of Pediatrics in Egypt.
Abstract:
Ultrasound techniques have been developed since the past century and are becoming more useful in different areas of medical knowledge. More recently, lung ultrasound gained importance throughout artefact analysis to help clinical evaluation at bedside and became subject of interest in the pediatric intensive care and emergency department settings for both procedural and diagnostic purposes. The normal pattern of lung ultrasound is defined by the presence of lung sliding associated with A-lines whereas B-lines may be representative of pathology findings. This review focuses on some of the most common pulmonary conditions, their respective sonographic features and clinical implications in the emergency department and pediatric intensive care unit. There have been a number of recent advancements in the field of point-of-care ultrasound, including lung ultrasound for pediatric populations. Evidence-based guidelines on the use of point-of-care lung ultrasound have been published. Lung ultrasound is superior to chest radiography in diagnosing several disorders. Before performing lung ultrasound, it is important to note that the position of the patient could affect the findings, as air increases and liquid sinks under the influence of gravity, lung ultrasound is usually performed with the patient in the supine position. While lung consolidation or pleural effusion is predominantly found in dependent and dorsal lung regions, pneumothorax is primarily found in the anterior chest.
Aim:
- We aim to review the application of lung ultrasound in bedside clinical medicine and introduce it as an adjunct to the stethoscope in physical examination.
- We review the basic points required to introduce lung ultrasound to physicians.
- We also aim to review the utility and application of lung ultrasound in pleural and parenchymal lung pathologies and also cover the use of ultrasound in thoracic procedures.
- To identify lung US artifacts in normal and abnormal thoracic examination
- To review and evaluate pneumothorax.
- General Pediatrics|Pediatric Pulmonology |Family Medicine | Neonatal Intensive Care Unit
Location: MENA Plaza Hotel Albarsha | Dubai, UAE

Chair
Brankica Vasiljevic
NMC Royal Hospital DIP, UAE
Session Introduction
Jose Arnold Tariga
Salma Children’s Rehabilitation Hospital, UAE
Title: The PALM initiative: The pediatric adaptation via learning modules initiative

Biography:
Jose Arnold Tariga has completed his Doctor of Philosophy in Development Education from Central Luzon State University, Philippines in 2019, Professional Diploma in Healthcare Administration from the American University of Ras Al Khaimah, UAE in 2015, Master of Science in Nursing (Major in Medical-Surgical Nursing) degree from Cebu Normal University, Philippines in 2012 and Bachelor of Science in Nursing in 2008. He is a Certified Professional in Healthcare Quality and is also Certified American Heart Association Basic Life Support Instructor. He is currently working as a Clinical Resource Nurse in Salma Rehabilitation Hospital based in United Arab Emirates where he is leading the Education and Training Department of the entire facility. He has published his researches in peer-reviewed journals and has also presented in various international conferences in UAE. He is a Member of the National League of Nursing and Sigma Theta Tau International Honor Society of Nursing based in US. With his valuable contribution in the healthcare community in the United Arab Emirates, he was recognized as the Healthcare Professional of the Year 2019 by The Filipino Times Awards in UAE.
Abstract:
Introduction & Aim: Nursing shortage is now becoming a global phenomenon with a projected need of 1.09 million nurses by 2024 in the US and a current shortage of 42,000 nurses in UK. According to DoH (2017), UAE will require 16,158 nurses by 2025. With the aim of developing a more sustainable solution for nursing shortage, the researcher developed a pediatric learning module to upskill adult-trained nurses and conducted this study to determine its effectiveness.
Method: The researcher utilized Solomon 4-Group Design to determine who will be assigned to receive the pretest, module and posttest. Data was collected using a test questionnaire and competency assessment checklists. Results were subjected to descriptive statistics and factorial analysis of covariance to assess if the demographic variables affect their level of knowledge and competency.
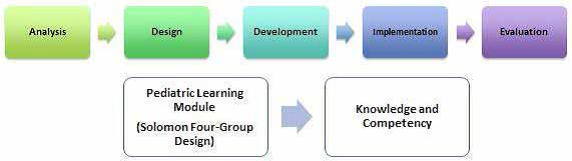
Figure 1: Module Development using ADDIE Model and the use of Solomon 4-Group Design to enhance knowledge and competency
Result: Results revealed that the module was successfully developed using the five stages of ADDIE Model namely: Analysis, Design, Development, Implementation and Evaluation. Majority of the respondents are married Asian females in their early adulthood, holding bachelor’s degree in nursing, with less than 5 years of experience. Factorial analysis revealed that demographic variables did not influence their level of knowledge and competency (p>0.5). The study also showed that the mean knowledge and competency levels of adult-trained nurses who received the module are significantly higher compared to those who did not undergo the module. Furthermore, the study revealed that there is a significant difference on the knowledge and competency levels between adult-trained nurses who used and did not use the pediatric module.
Conclusion: The Pediatric Adaptation via Learning Modules (PALM) initiative is effective in upskilling the skills and knowledge of nurses.
Preetha Gopinathan Nair Sajidammal
International Institute of Health Management Research, India
Title: Health care seeking for seriously ill newborns among families in the state of Haryana in India

Biography:
Preetha Gopinathan Nair Sajidammal is an Associate Professor in International Institute of Health Management Research, India. She teaches Epidemiology, Research Methodology and Health Systems to the students of MBA Health Management. Her interest areas are non-communicable diseases and perinatal/ neonatal survival. She has led and been part of many research projects in public health. She has developed many research reports, case studies and scientific publications.
Abstract:
Low costs, high impact focussed interventions have been identified to improve neonatal survival. This paper assesses the health seeking for sick newborns who were declared seriously ill immediately after their birth and the constraints faced by the families to access care. The study was done as a social autopsy of a sample of 382 neonatal deaths which occured during a calendar year (January- December 2017) in four districts (Jhajjar, Rewari, Rohtak and Hissar) of Haryana in India.
Using a semi structured social autopsy tool, information on the final illness of the newborn was collected from the principal care taker. It was seen that 75% of the total sample of newborns (287/382), 60% of them males, were recognized to be seriously ill at or immediately after birth; 39% of them (113/287) died in the hospitals they were born or reached after delivering out of hospital. Majorities were early neonatal deaths, pre term and had low birth weight. Three quarters of them could not be breastfed. The most common reasons for referral to higher facilities were need for specialized care or lack of equipment or drugs or oxygen administration facilities or blood transfusion facilities.
Treatment was delayed for many newborns due to time taken in reaching the referral facilities. Families had to bear high out of pocket expenditure and had to overcome challenges of cost among others. It is imperative that intensive care facilities for newborns are strengthened at secondary and tertiary levels of care, also ensuring availability of drugs and equipment.
Deepu Abraham
Zulekha Hospital, UAE
Title: Kawasaki disease – Challenges in diagnosis and management

Biography:
Deepu Abraham is a Consultant Pediatrician and Neonatologist working at Zulekha hospital Dubai. He did his post-graduation and MD in Pediatrics from Kerala, India. He did his further Pediatrics and Neonatology subspecialty training from Midlands and London Hospitals in UK completing his CCT in pediatrics and neonatology. He has presented papers in multiple national and international conferences. His areas of interests include long term follow up of chronic lung disease and associated cardio pulmonary complications.
Abstract:
Kawasaki disease (KD) is one of the most common vasculitides of childhood. It is in fact the most common cause of acquired heart disease in childhood in the developed world. The underlying pathology is infiltration of inflammatory cells into vascular tissue resulting in predominantly medium-sized artery vasculitis with a predilection for the coronaries.
There are many diagnostic challenges for KD. These include absence of confirmatory laboratory or imaging investigations, dependence on clinical criteria to diagnose and the fact that presentation is often “incomplete”, especially in infant age group. The primary goal in KD treatment is to reduce inflammatory response early in the disease course there by preventing coronary complications.
The mainstay of treatment for KD is IVIG (Intra Venous Immunoglobulin) and aspirin therapy. However, there is an increasing incidence of patients who do not respond to IVIG therapy. The incidence of coronary complications is significantly higher in the refractory KD group of children. This presentation is looking into the diagnostic challenges and management options in refractory KD cases.
Dhruba Shrestha
Siddhi Memorial Women and Children Hospital, Nepal
Title: Incidence and clinical profile of pneumonia in children before and after the introduction of PCV-10 vaccination in Bhaktapur, Nepal

Biography:
Dhruba Shrestha has completed his MBBS from BP Koirala Institute of Health Sciences, Nepal and MD in Pediatrics from National Academy of Medical Sciences, Nepal. His special interest is in pediatric nutrition and non-invasive cardiology. He has done his special Postgraduate Diploma in Pediatric Nutrition from Boston University, USA. He has many publications in international and national journals. He is also an Executive Committee Member of Nepal Pediatric Society (NEPAS).
Abstract:
Streptococcus pneumoniae is considered as the leading cause of Pneumonia, Meningitis, Otitis media, Sinusitis and Septicaemia. WHO also estimates that 1 in every 20 children below 5 years of age will have an episode of pneumonia each year. S pneumoniae is the most important cause of pneumonia in young children. Pneumococcal Conjugate Vaccine (PCV) have shown efficacy against several serotypes of S. pneumoniae and it is now part of routine immunization schedule in many countries, including Nepal. PCV-10 was first introduced in Nepal on 18th January 2015 and is now included in National Immunization Schedule at 6 weeks, 10 week and 9 month of age.
This was a retrospective study conducted in the pediatric unit of Siddhi Memorial Women and Children’s Hospital. Data was reviewed from January 2014 to December 2018. There were altogether 601 children admitted due to pneumonia in the study period after exclusion 593 cases were eligible for analysis. 63% had diffuse involvement of lung in X-ray. PCV 10 was introduced in our hospital in October 2015 and there is significant decrease in the admission due to pneumonia after its introduction.
Most commonly used antibiotics were Crystalline Penicillin and Cefotaxime for treatment and both were equally efficacious. Failure rates were 8% and 1% respectively. To conclude, PCV is a very effective vaccine for S. pneumoniae. There has been dramatic decrease in the incidence of pneumonia since its introduction. Penicillin is still an effective drug for treatment of pneumonia.
Magina Artikova
Tashkent Pediatric Medical Institute, Uzbekistan
Title: Secondary oxalate nephropathy in children with allergic pathology

Biography:
Magina Artikova studied at school Number 6 in Bukhara. From 2001 to 2008 she studied at Tashkent Pediatric Medical Institute (TPMI), faculty of pediatrics. From 2011 till 2017 she worked TPMI, assistant department Hospital pediatria. From 2018 till the present she has been working for researcher PhD at TPMI. Her scientific work is devoted to secondary oxalate nephropathy in children and the definition of disease development factors. She has studied the etiopathogenetic mechanisms of development of metabolic nephropathy in children, to develop a new methodology for effective therapy and prevent complication such uro and nephrolithiasis, urinary tract infection, chronic kidney disease.
Abstract:
Introduction & Aim: In recent years, there has been a steady increase in the number of children with hyperoxaluria along with various allergic pathologies. Hyperoxaluria is the main factor leading to the development of nephrolithiasis. The hyperoxaluria in children can be asymptomatic for a long time, leading to secondary oxalate nephropathy, urolithiasis and chronic kidney disease. Our objective was to assess the clinical features of patients with hyperoxaluria in combination with allergic pathology.
Materials & Methods: We observed 103 patients with secondary oxalate nephropathy (hyperoxaluria) aged 6 months to 7 years with a glomerular filtration rate above 60 ml/min. The median age of the patients was 3.48. All children underwent a general clinical examination: Oxalates in daily urine were determined, urine flow cytometry was performed, microalbumin in urine was determined, a general blood test, biochemical blood tests, determination of immunoglobulin E in the blood, bacteriological examination of feces for quantitative and qualitative composition of microflora were performed.
Results: Food allergies were identified in 18% of cases (9 patients), 7.7% of cases (8 patients) had urticaria, 23% (24 patients) had vasomotor rhinitis, 8.73% (9 patients) had atopic dermatitis. It was found that 28 children (27%) had a combination of allergic pathologies, such as vasomotor rhinitis and urticaria, atopic dermatitis and vasomotor rhinitis. In children with an existing allergic pathology, the clinical course of oxalate nephropathy was more pronounced than in children without allergic pathology. It was found that children with an aggravated allergic history were part of the often ill children group and therefore received frequent therapy with antibiotics in which the degree of hyperoxaluria was more pronounced, characterized by microalbuminuria and microhematuria.
Conclusion: The study showed that among children with hyperoxaluria a large number of children with allergic pathology were identified. Allergic pathology as a premorbid background often determines the peculiarity of the course of secondary oxalate nephropathy. In addition, the use of antibiotic therapy leads to a violation of the intestinal microbiome, which increases the risk of nephrolithiasis. Thus, allergopathology along with antibiotic therapy can be considered as risk factors for the adverse course of secondary oxalate nephropathy.
- Neonatal Care| Women Health Nursing and Midwifery | Pediatric Nutrition | Pediatric Surgery
Location: MENA Plaza Hotel Albarsha | Dubai, UAE

Chair
Amin Gohary
Burjeel Hospital, UAE
Session Introduction
Richa Prasad
The University of Manchester, UK
Title: Less is more! - A study of fluorosis in children and treatment with ICON, A novel minimally invasive treatment

Biography:
Richa Prasad has been practicing as a dentist with special interest in Aesthetic and Restorative Dentistry, and provision of Botox and fillers, and Invisalign Orthodontics. In clinical practice, situations where young children have a low self-esteem due to the appearance of their teeth is common and often overlooked due to the empirical advantage of water fluoridation in oral health. This study and review of literature should highlight the less publicised downside of community water fluoridation and also points towards the innovative treatment methods that should be adopted to minimise the aesthetic impact on young children.
Abstract:
Introduction: Modern methods of caries control are individual and community based. Fluoridation of community water supplies was started as an efficient and costeffective way to reduce caries in the population. It has been named as one of the 10 great public health achievements of the 20th century. However, with fluoride being more widely used in most dental products, the incidence of dental fluorosis appears to be on the rise. Traditional treatment for these white spot lesions has been highly invasive and not indicated in children. Low-viscosity resin-based materials are now proving to be game changers!
Aim: To assess the impact of water fluoridation on aesthetic appearance of teeth in children up to the age of 10 years and treatment with ICON resin infiltration.
Methods: Dean’s and Thylstrup and Fejerskov Fluorosis Index (TFI) was used to classify the degree and severity of fluorosis. A cross-sectional study was carried out among children along with review of literature about the incidence, effect and severity of dental fluorosis with community water fluoridation. Finally, treatment of dental fluorosis with minimally invasive methods for aesthetic improvement of the teeth was explored.
Results: ICON treatment is predictable (with case selection), is micro-invasive, and is a long lasting aesthetic solution that can be offered to growing children.
Conclusion: Awareness of fluoride intake with dental products, dietary fluoride and community water fluoridation is essential to prevent dental fluorosis. The advent of minimally invasive methods to treat white spot lesions has brought aesthetic treatment to children and is a valid micro-invasive alternative compared with traditional methods.
Saraswati Budhathoki Shrestha
Siddhi Memorial Women and Children Hospital, Nepal
Title: Serum vitamin D Status in pregnant women and their babies in Bhaktapur, Nepal

Biography:
Saraswati Budhathoki Shrestha has completed her Certificate Nursing from Madan Bhandari Memorial Nursing Campus, Bhadrapur, Nepal and Bachelor of Nursing from B.P. Koirala Institute of Health Sciences, Dharan, Nepal. She has worked in different hospitals of Nepal as a Nurse and also has experience in clinical research.
Abstract:
Vitamin D deficiency has been observed worldwide in pregnant women and their neonates. Maternal vitamin D deficiency can lead to deficiency in their newborn baby. It has been linked with various complications during pregnancy and delivery. There is risk of premature delivery and it is even linked with high neonatal mortality.79 pregnant women who came for delivery in the Siddhi Memorial Women and Children Hospital and their babies, after birth, were enrolled for the study. Maternal blood samples and umbilical cord blood samples of their babies were taken for the measurement of serum vitamin D and calcium level. Mean serum vitamin D and calcium level of pregnant mother before delivery were 14.67 ng/dl (8.5 SD) [95% CI (12.77- 16.58)] and 8.07 mg/dl (0.5 SD) [95% CI (7.89-8.26)] respectively. Similarly, the levels in the cord blood was 25.71 ng/dl (11.2 SD) [95% CI (23.23-25.81)] and 8.69 mg/dl (0.9 SD) [95% CI 8.48-8.89] respectively. Eighty-one percent (81%) of the mothers and 35.8% of their babies were found to have vitamin D deficiency. Although 97.5% of the pregnant women were taking calcium supplementation, serum calcium level was found to be lower than the normal reference value in 67% of the pregnant women and 64.2% of their babies. The study showed a positive correlation between the maternal and baby’s serum levels of vitamin D and calcium (p<0.001). There is high prevalence of vitamin D and calcium deficiency in pregnant mothers and newborn babies. Regular assessment of vitamin D and calcium level is essential during the pregnancy and pregnant women need to be supplemented with adequate amounts of these nutrients.
Magina Artikova
Tashkent Pediatric Medical Institute, Uzbekistan
Title: The role of Oxalobacter formigenes in the development of secondary oxalate nephropathy in children

Biography:
Magina Artikova studied at school Number 6 in Bukhara. From 2001 to 2008 she studied at Tashkent Pediatric Medical Institute (TPMI), faculty of pediatrics. From 2011 till 2017 she worked TPMI, assistant department Hospital pediatria. From 2018 till the present she has been working for researcher PhD at TPMI. Her scientific work is devoted to secondary oxalate nephropathy in children and the definition of disease development factors. She has studied the etiopathogenetic mechanisms of development of metabolic nephropathy in children, to develop a new methodology for effective therapy and prevent complication such uro and nephrolithiasis, urinary tract infection, chronic kidney disease.
Abstract:
Introduction: Hyperoxaluria is the main factor leading to the development of nephrolithiasis. Hyperoxaluria in children can be asymptomatic for a long time, leading to secondary oxalate nephropathy, to urolithiasis and chronic kidney disease. The vast majority of kidney stones are calcium oxalate.
Limiting the intake of products containing oxalic acid is not the main way to prevent calcium oxalate microlites. In this regard, scientists were interested in the bacterium Oxalobacter formigenes, which exhibits a symbiotic relationship with the human body by reducing the absorption of oxalates in the intestinal lumen with a further decrease in their concentration in plasma and urine. Oxalobacter formigenes is currently the most effective intestinal absorbent microbial oxalate.
Objective: To determine the species and quantitative composition of intestinal microflora and Oxalobacter formigenes in feces in children with secondary oxalate nephropathy, who had a history of antibiotic therapy.
Materials & Methods: 35 children with secondary oxalate nephropathy (hyperoxaluria) aged 6 months to 7 years with a glomerular filtration rate above 90 ml/min were observed. The median age of the patients was 3.48. Children were divided into two groups: The main and control. The control group consisted of 10 children with secondary oxalate nephropathy with no history of antibiotic therapy. The diagnosis of secondary oxalate nephropathy was made according to the classification developed by M. S. Ignatova et al. and N.V. Voronina: moderate hyperoxaluria, pronounced oxalate-calcium crystalluria, microhematuria and/or proteinuria, increased microalbumin in the urine (tubular dysfunction). All children underwent a general clinical examination: Oxalates in daily urine, microalbumin in urine, bacteriological examination of feces for quantitative and qualitative composition of microflora, PCR identification of Oxalobacter formigenes in feces were determined. The severity of dysbiotic changes in the intestines in the examined children was determined taking into account the Industry standard 91500.11.0004-2003 “Protocol for the management of patients intestinal dysbiosis”.
Results: The results showed that all children in the main study group had higher levels of oxalate in daily urine of 1.2 mg/kg/ day (at a rate of 0-0.5 mg/kg/day) than in the comparison group (0.5 mg/kg/day). Gross or microscopic hematuria is found in 65% to 90% of children who have urolithiasis. All children in the main group showed a violation of the quantitative and qualitative composition of the intestinal microbiota. In the comparison group, no signs of intestinal microbiota disturbance were noted. Grade 2 dysbiosis predominated in severity in 18 children, in 2 children dysbiosis of 3 degrees was detected, in 4 children dysbiosis of 1 degree was noted. In 6 children with secondary oxalate nephropathy, Oxalobacter formigenes was not detected. It was found that children in whom Oxalobacter formigenes was not determined received a history of antibiotics of the 3rd generation cephalosporins group, Co-trimaxazole, more than 6 times for 12 months. In 21 children, Oxalobacter formigenes has been identified.
Conclusion: In most cases, in children with secondary oxalate nephropathy, the use of antibiotics was detected and a violation of the intestinal microbiota was found. In 5 children, Oxalobacter formigenes was not identified in feces.








